Peptic Ulcer Treatment: A Complete Healing Guide
That sharp, burning, or gnawing pain in your upper stomach—is it just acidity, or something more? For millions of Indians, this discomfort is a daily reality, and it's often the first sign of peptic ulcer disease. A peptic ulcer is more than just discomfort; it's an open sore in the lining of your stomach or the upper part of your small intestine.
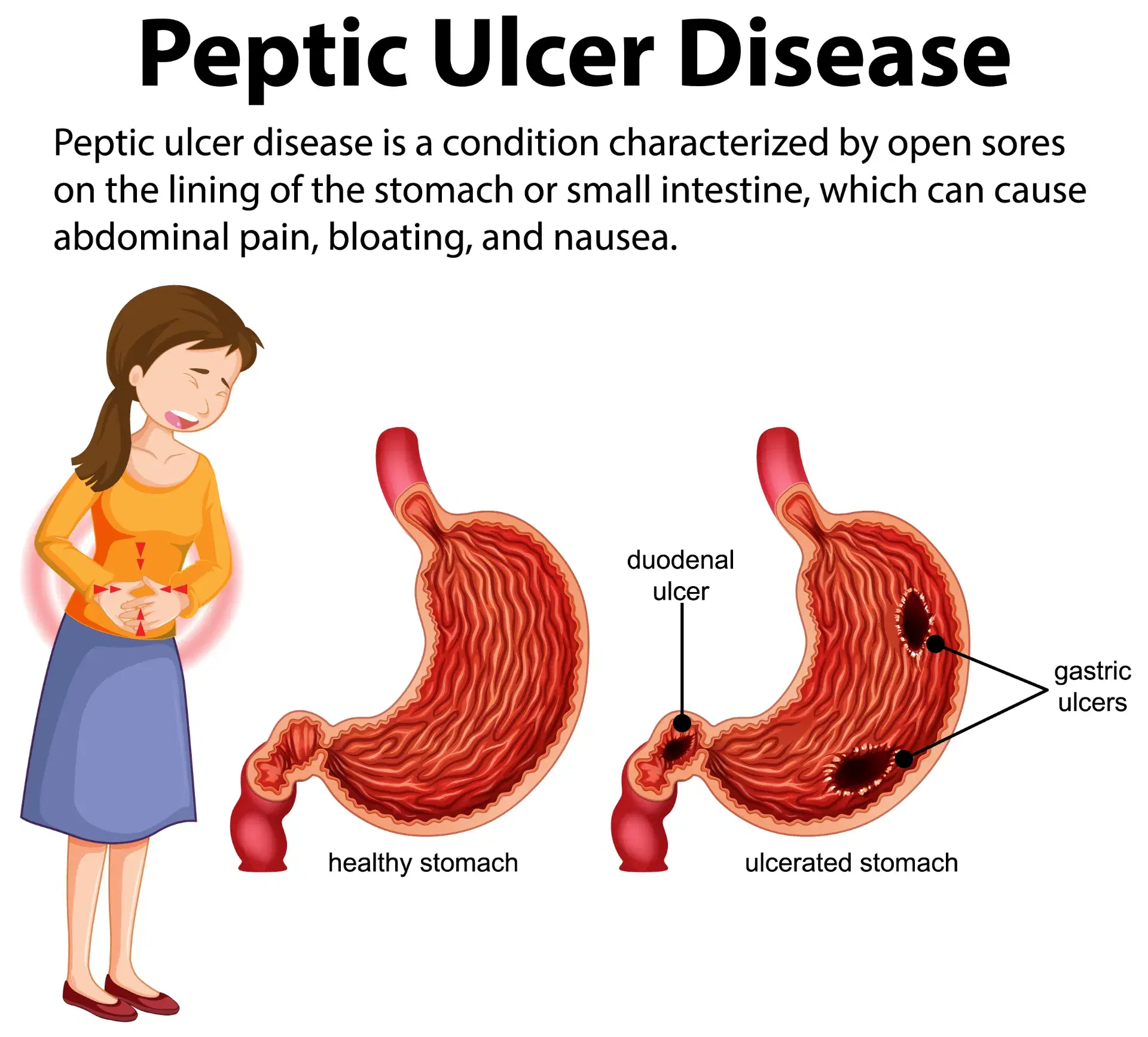
Understanding this condition is the first step toward healing. Peptic ulcers are broadly categorized into two main types: gastric ulcers (which occur inside the stomach) and duodenal ulcers (which occur in the duodenum, the first part of the small intestine). The most common causes are a persistent bacterial infection known as Helicobacter pylori (or H. pylori ulcers) and the long-term use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)—common painkillers many of us take for headaches and body aches.
It's very common for people to misdiagnose their digestive pain. For instance, the discomfort from an ulcer is often confused with other digestive issues, like the sharp, localized pain associated with Diverticulitis symptoms. However, these are vastly different conditions requiring different treatments. This comprehensive guide will walk you through everything you need to know about peptic ulcer treatment, from diagnosis and duodenal ulcer treatment to stomach ulcer healing, diet, and recovery timelines.
Understanding Peptic Ulcer Disease
A. What is a Peptic Ulcer?
Think of your stomach as a delicate pouch protected by a thick layer of mucus. This mucus shields the stomach wall from the strong acid your body produces to digest food. A peptic ulcer forms when this protective layer is damaged or worn away, allowing the acid to eat at the sensitive tissue underneath, creating a sore. It's much like a painful ghav or chhaala (wound) inside your digestive tract.
The key difference between the two types lies in their location and, often, their symptoms:
- Stomach (Gastric) Ulcer: Located on the inside lining of the stomach. Pain often feels worse after eating, as food and acid are churned together, irritating the sore.
- Duodenal Ulcer: Located in the duodenum. Pain might temporarily get better after eating (as food buffers the acid) but often returns with a vengeance 2-3 hours later when the stomach is empty.
B. Common Causes of Peptic Ulcer Disease
- H. pylori Ulcers: This is the leading cause worldwide, including in India. H. pylori is a spiral-shaped bacterium that can live in the sticky mucus layer of the stomach. It's incredibly resilient and can survive the harsh acidic environment. Over time, it causes inflammation (gastritis) and damages the protective lining, making it easy for an ulcer to form.
- NSAID Overuse: This is the second most common cause. Many people rely on over-the-counter painkillers like aspirin, ibuprofen (e.g., Brufen), or naproxen for chronic pain, arthritis, or headaches. Taken occasionally, they are generally safe. But used daily or in high doses for long periods, they can interfere with the stomach's ability to produce its protective mucus, leading to ulcers.
- Lifestyle Factors: While they don't typically cause ulcers on their own, these factors can worsen existing ulcers and dramatically slow down the healing process:
- Smoking: Nicotine increases stomach acid production and reduces the protective mucus, making you more susceptible.
- Alcohol: Excessive alcohol can irritate and erode the stomach lining.
- Stress: Severe physical or emotional stress doesn't directly cause an ulcer, but it can worsen the pain and make healing much more difficult by increasing acid secretion.
C. How Diverticulitis Symptoms Differ
It's crucial to distinguish peptic ulcer disease from other conditions. A common point of confusion is Diverticulitis symptoms. Diverticulitis is a condition of the large intestine (the colon). It occurs when small, bulging pouches (diverticula) that can form in the lining of your colon get inflamed or infected.
The symptoms are distinctly different:
- Peptic Ulcer: Pain is in the upper abdomen, typically a burning or gnawing feeling.
- Diverticulitis: Pain is usually sharp, persistent, and located in the lower-left side of the abdomen. It is often accompanied by fever, chills, and a significant change in bowel habits (like constipation or diarrhea).
Confusing the two can delay proper care, which is why a medical diagnosis is essential.
Signs & Symptoms of Peptic Ulcers
While the hallmark symptom is a burning stomach pain, peptic ulcer disease can manifest in several ways. The pain is often felt anywhere from your navel up to your breastbone.
Common signs include:
- Burning, gnawing, or aching pain: This is the most classic symptom.
- Bloating or a feeling of fullness: You might feel uncomfortably full after eating very little.
- Frequent belching (dakaar) or burping.
- Nausea and sometimes vomiting.
- Heartburn or acid reflux: A burning sensation that can travel up your chest.
- Intolerance to fatty foods.
As mentioned earlier, the timing of the pain can be a major clue:
- Stomach Ulcer: Pain often intensifies 1-2 hours after a meal.
- Duodenal Ulcer: Pain often appears 2-3 hours after a meal or wakes you up in the middle of the night on an empty stomach. Eating a small snack or drinking milk might provide temporary relief.
When Symptoms Become a Medical Emergency:
Do not ignore these "red flag" symptoms. Go to an emergency room immediately if you experience:
- Sudden, sharp, and severe stomach pain that doesn't go away. This could be a perforation (a hole).
- Vomiting blood: This may look bright red or like dark "coffee grounds."
- Black, tarry, or sticky stools (kaala mal): This is a sign of digested blood, indicating internal bleeding.
- Unexplained weight loss or difficulty swallowing.
Diagnosis: How Doctors Confirm Peptic Ulcer Disease
To provide the right treatment, your doctor must confirm you have an ulcer and find its cause. Guesswork isn't enough.
- Upper GI Endoscopy (EGD): This is the gold standard for diagnosis. A gastroenterologist uses a thin, flexible tube with a tiny camera on the end (an endoscope) to look directly at your esophagus, stomach, and duodenum. This allows the doctor to see the ulcer, assess its size, and check for any bleeding.
- Biopsy: During the endoscopy, the doctor will almost always take a tiny tissue sample (biopsy) from the stomach lining. This sample is then tested in a lab for two crucial things:
- To detect the presence of H. pylori ulcers.
- To rule out any cancerous cells (which is rare, but a necessary check for stomach ulcers).
- H. pylori Tests (Non-invasive): If an endoscopy isn't immediately performed, your doctor might use other tests to check for H. pylori:
- Urea Breath Test: A simple and highly accurate test where you drink a special solution and then breathe into a bag.
- Stool Antigen Test: This test checks your stool sample for proteins associated with the H. pylori bacterium.
Based on these findings, a clear treatment plan for your peptic ulcer disease can be created.
Section Highlight: Differentiating Peptic Ulcer Pain from Diverticulitis Symptoms
One of the greatest challenges in self-diagnosing digestive pain is the sheer number of conditions that feel similar. As we've touched on, a primary source of confusion is mistaking ulcer pain for Diverticulitis symptoms. Let's break down this comparison, as understanding the difference is vital for seeking the right help.
Peptic Ulcer Symptoms (A Recap):
- Primary Location: Upper abdomen, between the breastbone and the navel (also called the epigastric region).
- Nature of Pain: Typically a burning, dull, or gnawing ache. It's often described as a "hunger pang" that won't go away.
- Timing: Directly related to your eating schedule. It either gets worse after eating (stomach ulcer) or appears 2-3 hours after eating on an empty stomach (duodenal ulcer).
- Associated Symptoms: Bloating, belching, nausea, and heartburn. Fever is extremely rare unless a complication like perforation occurs.
Diverticulitis Symptoms (The Contrast):
- Primary Location: Lower-left abdomen. This is the most common site because this part of the colon (the sigmoid colon) is where diverticula most frequently form.
- Nature of Pain: Usually a sharp, constant, and localized pain. The area is often very tender to the touch.
- Timing: Not typically related to meals. The pain is generally constant and persistent.
- Associated Symptoms: This is the key differentiator. Diverticulitis symptoms are often systemic, meaning they affect the whole body. This includes:
- Fever and chills (a sign of infection/inflammation).
- A marked change in bowel habits (sudden constipation or, less commonly, diarrhea).
- Nausea and vomiting.
- Abdominal tenderness.
Mistaking one for the other can lead to significant delays in care. Treating the potential infection from Diverticulitis symptoms (which often requires antibiotics and rest) is a completely different protocol from the acid-reduction and bacterial eradication needed for peptic ulcer disease. This is why you should never ignore persistent abdominal pain. A gastroenterologist can perform the right tests to pinpoint the exact cause and ensure you're not treating the wrong condition.
Treatment Options for Peptic Ulcers (Core Section)
The good news is that peptic ulcers are highly treatable. The treatment plan will depend entirely on the cause of your ulcer.
A. Medications for Stomach Ulcer Healing
If your ulcer is not caused by H. pylori (e.g., it's from NSAID use), the primary goal is to reduce stomach acid and allow the ulcer to heal.
- Proton Pump Inhibitors (PPIs): These are the most powerful acid-reducing drugs. Names like Omeprazole, Pantoprazole ("Pantop"), Esomeprazole, and Rabeprazole are extremely common in India. They work by blocking the tiny "pumps" in your stomach cells that release acid. This creates a low-acid environment, giving the ulcer time to heal.
- H2-Receptor Blockers: These drugs, like Famotidine, also reduce stomach acid, though they are generally less potent than PPIs. They work by blocking histamine, a signal that tells your stomach to produce acid.
- Mucosal Protective Agents: These medicines work differently.
- Sucralfate: This medication forms a protective "bandage" or coating over the ulcer, shielding it from acid and enzymes while it heals.
- Bismuth Subsalicylate: This can also help coat the ulcer and has some antibacterial effects.
B. Duodenal Ulcer Treatment (and H. pylori Ulcers)
If your diagnosis confirms H. pylori ulcers, the treatment plan has a different priority: eradicate the bacteria. If you don't kill the bacteria, the ulcer will almost certainly come back.
- Eradication Therapy: This involves a combination of medications, often called "triple therapy" or "quadruple therapy," taken for 10 to 14 days.
- The typical combination includes:
- A PPI (like Omeprazole) to reduce acid.
- Two or three antibiotics (common ones include Amoxicillin, Clarithromycin, and Metronidazole) to kill the H. pylori bacteria.
- It is absolutely essential to take the full course of antibiotics, even if you start feeling better. Stopping early is a primary reason for treatment failure and can lead to antibiotic resistance. This is the most critical step in learning how to cure stomach ulcer caused by H. pylori.
C. Lifestyle & Habit Changes
Medication alone is often not enough. Your lifestyle must support the healing process.
- Stop Smoking: This is non-negotiable. Smoking slows stomach ulcer healing and is linked to ulcer recurrence.
- Reduce or Eliminate Alcohol: Alcohol is a direct irritant to the stomach lining.
- NSAID Review: Stop taking NSAIDs. If you need painkillers for another condition, talk to your doctor. Paracetamol is usually a-safe alternative.
- Stress Management: While not a direct cause, managing stress through yoga, meditation, deep breathing, or simple hobbies can prevent excess acid production and support your body's healing.
D. When Surgery Is Required
In today's medical landscape, surgery for ulcers is rare. It's reserved for emergency complications, such as:
- An ulcer that has perforated (torn) the stomach or duodenal wall.
- An ulcer that is causing severe, uncontrollable bleeding.
- An ulcer that has caused scar tissue to block food from leaving the stomach (gastric outlet obstruction).
PROMINENT Q&A SECTION (Answer Engine Optimized)
Let's answer the most common questions patients have about peptic ulcer disease.
1. How long do ulcers take to heal?
This is the most frequent question, and the answer depends heavily on the cause and on you.
With proper medical treatment, most uncomplicated gastric (stomach) ulcers heal in 6 to 8 weeks. Uncomplicated duodenal ulcers often heal faster, typically in 4 to 6 weeks.
However, this timeline for stomach ulcer healing and duodenal ulcer treatment is affected by several factors:
- The Cause: If your ulcer is from NSAID use, it will start to heal very quickly once you stop the medication and start a PPI. If it's from H. pylori ulcers, healing is entirely dependent on successfully eradicating the bacteria.
- Size and Severity: A large, deep, or bleeding ulcer will naturally take longer to heal than a small, superficial one.
- Treatment Compliance: This is the biggest factor you control. If you skip your PPI doses or don't finish your 14-day antibiotic course, you are constantly interrupting the healing process. You must take your medication exactly as prescribed.
- Lifestyle: If you continue to smoke, your ulcer may take twice as long to heal—or it may not heal at all. Drinking alcohol will also delay recovery.
- Follow-Up: For a gastric (stomach) ulcer, your doctor will likely schedule a repeat endoscopy after 8-12 weeks to visually confirm that the ulcer has healed completely. This is a crucial step to ensure the stomach ulcer healing is complete and to re-check for any underlying issues. For a duodenal ulcer, a follow-up breath or stool test to confirm H. pylori is gone is more common.
2. Can ulcers heal without treatment?
This is a dangerous misconception. The simple answer is no, not really, and it's incredibly risky to try.
An ulcer is not like a simple scrape on your skin. It's an open wound in a highly acidic, hostile environment. While the pain from an ulcer might come and go—you might feel better for a few days—the underlying wound is still there. Drinking milk or taking an over-the-counter antacid might neutralize the acid for a few minutes and temporarily ease the pain, but this does nothing to heal the actual sore.
Ignoring peptic ulcer disease or trying to "wait it out" is a gamble. Untreated ulcers, especially H. pylori ulcers, can lead to severe, life-threatening complications:
- Bleeding: The ulcer can erode into a blood vessel, causing bleeding that can range from slow (leading to anemia, fatigue, and weakness) to rapid and massive (causing vomiting of blood and requiring emergency hospitalization).
- Perforation: The ulcer can eat completely through the wall of the stomach or duodenum, spilling digestive acids and food into the abdominal cavity. This causes sudden, excruciating pain and is a life-threatening emergency (peritonitis) that requires immediate surgery.
- Obstruction (Blockage): Over time, a chronic ulcer can create scar tissue that swells and blocks the normal passage of food. This can cause persistent vomiting, a feeling of being full, and weight loss.
Therefore, self-treating with antacids is like putting a tiny bandage on a deep wound. You are not fixing the problem, you are only masking the pain while the underlying damage gets worse.
3. What foods heal ulcers?
Let's be very clear: No single food will cure an ulcer. An ulcer is a medical condition that requires medication. However, your diet plays a massive role in creating the best possible environment for stomach ulcer healing.
The goal of an "ulcer-friendly" diet is twofold:
- Avoid foods that irritate the wound and increase acid production.
- Include foods that support the gut lining and may even help combat H. pylori.
Foods to Include (The "Good List"):
- Probiotics: These are the "good" bacteria that help balance your gut. Foods like dahi (plain curd), yogurt (with live cultures), and buttermilk (chaas) can be very beneficial. Some research suggests probiotics can make H. pylori treatment more effective and reduce antibiotic side effects.
- Fiber-Rich Foods: Soluble fiber, in particular, can be helpful. Good sources include oats, barley, psyllium husk (isabgol), apples, and bananas.
- Soothing Foods: These are easy to digest and gentle on the stomach. Think of khichdi (made with minimal spice), boiled potatoes, plain rice, and steamed vegetables. Coconut water (nariyal pani) is excellent for hydration and is very gentle.
- Flavonoid-Rich Foods: Flavonoids are compounds found in plants that can have anti-inflammatory and protective effects. Good sources include apples, berries, and green tea (though be mindful of the caffeine).
- Cabbage: Cabbage juice is a traditional remedy for ulcers. While it doesn't sound tasty, cabbage is rich in Vitamin C and an amino acid called glutamine, which are thought to help support the mucosal lining.
Integrating Overall Gut Health:
It's not just about the stomach; it's about your entire digestive tract. As discussed by Bangalore Gastro Centre experts in the video, "Eat These Fantastic Foods for a Healthy Small Intestine!", focusing on foods that nourish your gut is key to long-term digestive wellness. A healthy small intestine (where duodenal ulcers occur) is vital for absorbing the nutrients your body needs to repair itself. Foods that are easy to digest and rich in supportive nutrients contribute directly to your body's ability to heal from peptic ulcer disease.
How to Cure Stomach Ulcer Completely (Step-by-Step Strategy)
Figuring out how to cure stomach ulcer or duodenal ulcer treatment for the long term isn't about a single magic pill. It's a multi-step strategy that requires a partnership between you and your doctor.
Step 1: Get a Precise Diagnosis.
Stop guessing. Don't assume your pain is just "gas" or "acidity." Go to a doctor, preferably a gastroenterologist. Get the endoscopy and the H. pylori test. You must know the exact cause of your ulcer. Is it H. pylori ulcers or is it from painkillers? The entire treatment plan hinges on this one question.
Step 2: Follow Your Medication Plan Religiously.
This is the most important step.
- If you have H. pylori: You must complete the full 10-14 day course of antibiotics. Do not stop on day 8 just because you feel better. If you do, the bacteria can return, and they may come back resistant to the antibiotics, making your next treatment much harder.
- Take your PPI correctly: PPIs are most effective when taken 30-60 minutes before your first meal of the day (e.g., before breakfast). This allows the medicine to block the acid pumps before they get activated by food.
Step 3: Commit to a 6-8 Week "Ulcer-Friendly" Diet.
While your ulcer is healing, you must be strict. This is a temporary sacrifice for long-term health.
- NO Spicy Foods: This means no red chilli powder, garam masala, green chillies, or very hot curries.
- NO Oily/Fatty Foods: Avoid deep-fried items like samosas, pakoras, vadas, and heavy, oily gravies. Fat slows down stomach emptying, giving acid more time to cause trouble.
- NO Caffeine: This includes coffee, strong black tea, and colas. These are direct acid stimulants.
- NO Alcohol: Not even beer or wine. Alcohol is a direct irritant that will prevent healing.
- NO Smoking: This is non-negotiable.
- YES to simple, home-cooked, low-spice meals. Think idli, dosa (with mild sambar), khichdi, dahi-rice, boiled vegetables, and grilled (not fried) fish or chicken.
Step 4: Confirm the Cure.
Feeling better isn't the same as being cured. Once your treatment course is done, your doctor will schedule a follow-up.
- For H. pylori ulcers, this will likely be a breath test or stool test a few weeks later to confirm the bacteria are 100% gone.
- For a stomach ulcer, this may be a repeat endoscopy to visually confirm the wound is closed.
This is the only way to truly know you have learned how to cure stomach ulcer and that it's not just hiding.
Step 5: Practice Relapse Prevention.
Once you are healed, you can slowly reintroduce foods. But you must remain vigilant. Avoid long-term NSAID use forever. If you get arthritis or body pain, ask your doctor for safer alternatives. If you feel the early warning signs (that familiar gnawing pain) returning, see your doctor immediately.
Long-Term Care & Prevention
For many people, a peptic ulcer is a one-time event that, once treated, is gone for good. But for others, especially those with a history of recurrent ulcers, long-term vigilance is key.
- Be Mindful of Painkillers: This is the most important preventive measure. For any future aches and pains, make paracetamol your first choice. If a doctor must prescribe an NSAID for a condition like arthritis, make sure they know your ulcer history. They will almost always co-prescribe a PPI to protect your stomach.
- Don't Ignore Symptoms: If you've had peptic ulcer disease before, you know what it feels like. If those symptoms return, don't try to self-treat for weeks. See your doctor right away.
- Manage Your Digestive Health: Your digestive system is a complex, interconnected environment. Managing chronic conditions is a holistic process. This applies whether you are dealing with peptic ulcer disease or other inflammatory conditions like Crohn's Disease: Symptoms, Treatment & Management Strategies.
When to Consult a Gastro Specialist
Your family doctor or a general physician can often manage a straightforward case of peptic ulcer disease. However, you should see a gastroenterologist (a specialist in digestive diseases) if:
- Your symptoms are severe.
- You have any of the "red flag" symptoms mentioned earlier (bleeding, black stools, severe pain).
- Your symptoms don't get better after the standard course of treatment.
- You have a recurrent ulcer that keeps coming back.
A specialist is essential in these cases. Specialized centers, such as Bangalore Gastro Centre, are equipped with high-definition endoscopy suites and advanced diagnostic tools. This allows for the most precise diagnosis and the creation of a tailored treatment plan, especially for complex or stubborn cases.
Conclusion: Your Path to Healing
The pain of peptic ulcer disease can be frightening and disruptive, but it is important to remember that this is one of the most treatable conditions in all of gastroenterology. Healing is not just possible; it's highly probable.
Your recovery stands on a "tripod" of three essential legs:
- Medical Treatment: Taking the right medications (PPIs and/or antibiotics) exactly as prescribed.
- Dietary Changes: Avoiding irritants and embracing soothing, healing foods.
- Lifestyle Modifications: Quitting smoking, reducing alcohol, and managing stress.
If any one of these legs is weak, the healing process can be slow or incomplete.
Don't ignore persistent stomach pain. Don't write it off as "just acidity," and don't confuse it with other issues like Diverticulitis symptoms. Listen to your body, seek professional advice, and commit to your treatment plan. You can and will heal.
