Crohn's Disease: Symptoms, Treatment & Management Strategies
Crohn's disease, a perplexing and often debilitating condition, impacts countless lives across India and the globe. As a chronic inflammatory bowel disease (IBD), it doesn't just cause a fleeting stomach upset; it's a persistent, sometimes severe, inflammation of the digestive tract that can lead to significant discomfort and long-term complications if left unaddressed. Understanding Crohn's disease treatment and effective management is not merely beneficial, but vital for those affected to maintain a good quality of life.
This comprehensive guide aims to shed light on Crohn's disease, breaking down its intricate nature into easily digestible information. We'll explore everything from the subtle Crohn's symptoms that often get mistaken for other ailments to the underlying causes and triggers that can ignite a flare-up. More importantly, we'll delve deep into the various Crohn's disease treatment options available today, ranging from advanced medications to practical lifestyle and dietary adjustments. Our goal is to empower you with knowledge, offering actionable tips for managing Crohn's disease and answering common questions that patients frequently ask. At Bangalore Gastro Centre, we believe that education is the first step towards better gut health, and this blog is a testament to our commitment to helping you navigate complex digestive conditions like this inflammatory bowel disease.
What Is Crohn’s Disease and How Does It Affect the Body?
Q1: What is Crohn’s disease?
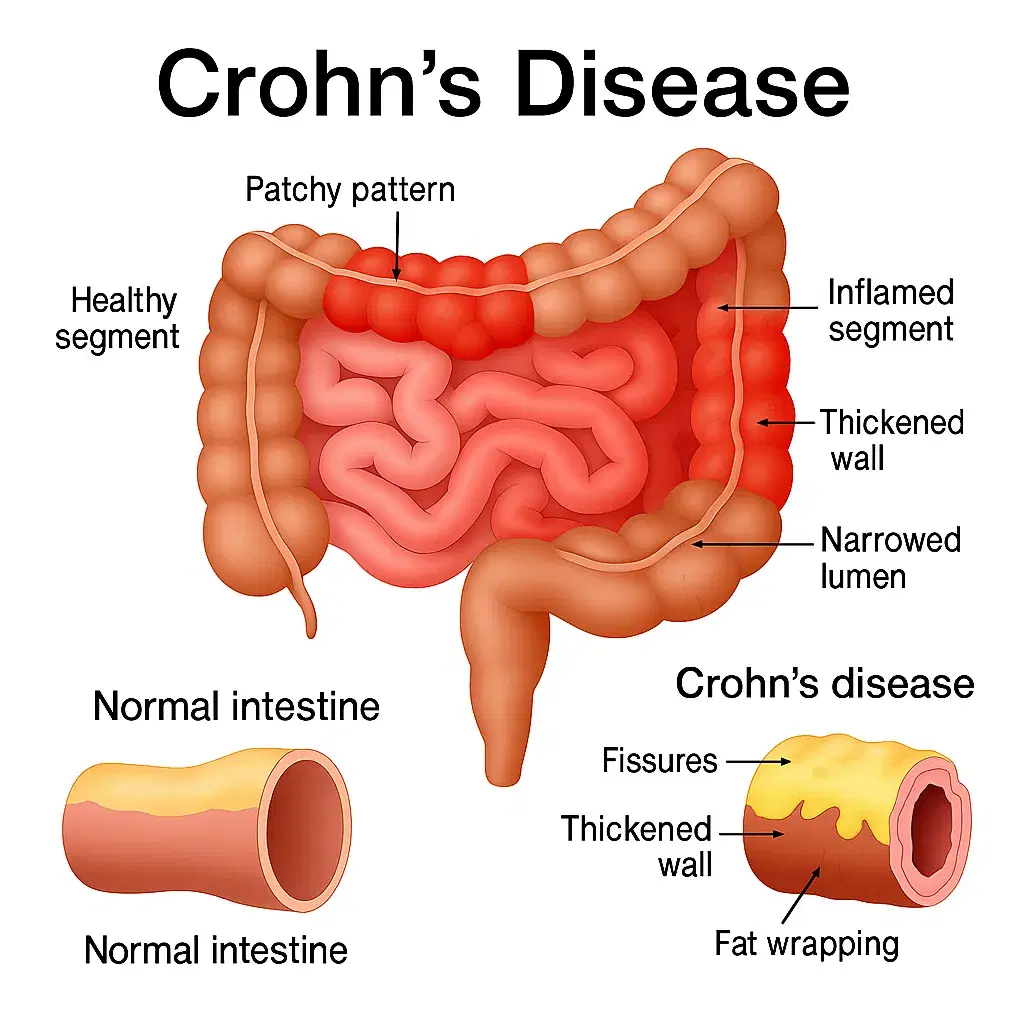
Imagine your digestive system, a long tube designed to process food, absorb nutrients, and eliminate waste, suddenly becoming a battlefield of inflammation. That's essentially what happens with Crohn's disease. It's a chronic, long-term inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal (GI) tract, from the mouth right down to the anus. Unlike its close cousin, ulcerative colitis, which typically affects only the colon and rectum and involves continuous inflammation of the innermost lining, Crohn's disease is characterized by patchy areas of inflammation that can skip sections of the GI tract and penetrate all layers of the bowel wall. This deep inflammation can lead to a host of problems, including narrowing of the bowel, ulcers, and even tunnels (fistulas) to other organs or the skin. When Crohn's specifically affects the large intestine, it's known as Crohn's colitis.
Q2: Why is Crohn’s considered a type of inflammatory bowel disease?
The term "inflammatory bowel disease" itself provides a clue. It refers to a group of conditions characterized by chronic inflammation of the digestive tract. Crohn's disease fits this description perfectly because its core pathology involves an abnormal immune response. For reasons not fully understood, the body's immune system, which is supposed to fight off foreign invaders like bacteria and viruses, mistakenly attacks healthy cells in the GI tract. This misguided attack leads to persistent inflammation, which in turn causes the array of Crohn's symptoms experienced by patients, such as chronic diarrhea, severe abdominal pain, debilitating fatigue, and nutrient malabsorption that can result in significant weight loss. It's a complex interplay where the body's own defense mechanism turns against itself, creating a cycle of inflammation and damage.
Understanding Crohn’s Symptoms
Q3: What are the most common symptoms of Crohn’s disease?
The Crohn's symptoms can be quite varied, making diagnosis challenging, but certain signs are more prevalent. The primary symptoms often include:
- Abdominal Pain and Cramping: Often localized to the lower right abdomen (if the small intestine is involved), but can occur anywhere. It can feel like sharp pangs or a dull, persistent ache, sometimes worsening after meals, akin to a persistent, uneasy feeling after eating a rich Indian thali.
- Persistent Diarrhea: This is frequently watery and can be accompanied by urgency.
- Fatigue: A profound, often inexplicable tiredness that doesn't improve with rest, severely impacting daily activities.
- Weight Loss: Due to reduced appetite, malabsorption of nutrients, and the body's increased energy demands from fighting inflammation.
- Blood in Stool: Can be bright red (if near the rectum) or darker and mixed with stool.
Beyond these, secondary symptoms might include:
- Fever: Especially during active inflammation or flare-ups.
- Reduced Appetite: Making it difficult to eat enough to maintain weight.
- Mouth Sores: Canker sores or ulcers, sometimes indicating inflammation higher up in the GI tract.
- Joint Pain: Arthritis-like pain, often affecting large joints.
- Skin Inflammation: Red, tender nodules (erythema nodosum) or painful ulcers (pyoderma gangrenosum).
The location of the disease significantly influences the symptoms. For instance, if Crohn's affects the small intestine, malabsorption and weight loss might be more prominent. If it’s Crohn's colitis, affecting the colon, diarrhea and blood in the stool are more typical. Understanding these varied Crohn's symptoms is crucial for early detection and effective inflammatory bowel disease treatment.
Q4: Can Crohn’s symptoms mimic other digestive issues?
Absolutely. This is one of the primary reasons why diagnosing Crohn’s disease can be a prolonged process. The early Crohn's symptoms often overlap considerably with other common, less severe digestive issues. For instance, persistent abdominal pain and altered bowel habits are hallmarks of Irritable Bowel Syndrome (IBS), a functional disorder of the gut. Similarly, diarrhea after consuming dairy products can point to lactose intolerance, and chronic digestive upset combined with nutrient deficiencies might suggest celiac disease, a gluten-induced autoimmune condition. Even a simple stomach bug can present with similar acute symptoms.
Because of this mimicry, a definitive diagnosis of Crohn’s disease requires a thorough medical evaluation. This typically involves a combination of investigative procedures, including a colonoscopy to visualize the colon and terminal ileum (the last part of the small intestine), imaging studies like MRI or CT scans to assess inflammation and complications throughout the GI tract, and biopsies of inflamed tissue for microscopic examination. These specialized tests help differentiate Crohn's from other conditions and are crucial for initiating the correct Crohn's disease treatment.
Causes and Triggers — What Leads to Crohn’s Disease?
Q5: What causes Crohn’s disease?
The precise cause of Crohn’s disease remains elusive, but scientists believe it's a multifactorial condition, meaning it arises from a complex interplay of several factors rather than a single culprit. The prevailing theory suggests a combination of:
- Immune System Malfunction: As mentioned earlier, the immune system mistakenly attacks healthy cells in the GI tract, leading to chronic inflammation. It's like a security system designed to protect your home suddenly perceiving your own family members as intruders.
- Genetics: There's a genetic predisposition to Crohn’s. If you have a family member with IBD, your risk is slightly higher. This doesn't mean you'll definitely get it, but it suggests a genetic vulnerability.
- Environment: Environmental factors play a role, though specific triggers are still being researched. Westernized diets, hygiene practices, and even geographical location are thought to contribute.
- Gut Microbiota: The trillions of bacteria, fungi, and other microorganisms living in your gut (your gut microbiome) are crucial for health. An imbalance or dysbiosis in this microbial community is increasingly linked to the development of inflammatory bowel disease.
Lifestyle factors, while not direct causes, can also influence the disease. For instance, smoking is a significant risk factor for developing and worsening Crohn's disease.
Q6: What triggers Crohn’s flare-ups?
While there's no known single cause, identifying what triggers a "flare-up" is critical for managing Crohn's disease. A flare-up signifies a period of active inflammation and a worsening of Crohn's symptoms. It's like a dormant volcano suddenly erupting. Common triggers include:
- Stress: While stress doesn't cause Crohn's, it's a well-known instigator of flare-ups. The gut-brain axis ensures that emotional distress can manifest as physical symptoms in the digestive system.
- Certain Foods: Highly processed, fatty, or spicy foods, common in many Indian diets, can sometimes irritate the inflamed bowel and trigger symptoms. It's often a very personal list of trigger foods.
- Infections: Bacterial or viral infections in the gut can provoke an immune response that exacerbates Crohn's.
- Antibiotics: These medications, while necessary, can disrupt the delicate balance of the gut microbiome, potentially leading to flares.
- Smoking: A major aggravator of Crohn's disease, smoking increases the frequency and severity of flares and the need for surgery.
- Skipping Medication: Adherence to prescribed Crohn's disease treatment is paramount. Missing doses can quickly lead to a return of symptoms.
Understanding the connection between diet and the gut microbiome is vital here. A gut-friendly diet can significantly aid in managing Crohn's disease and reducing flare frequency. For more insights on this, you might find this video helpful: 👉 Eat These Fantastic Foods for a Healthy Small Intestine! This video, from the experts at Bangalore Gastro Centre, offers fantastic insights into gut-friendly foods that can support your digestive health.
Crohn’s Disease Treatment — Current Medical Options
Q7: What are the main treatment options for Crohn’s disease?
The core objective of Crohn's disease treatment is to reduce inflammation, alleviate symptoms, and achieve long-term remission, preventing complications. This typically involves a multi-pronged approach, tailored to the individual's disease severity and location.
Medical Management:
- Anti-inflammatory Drugs:
- Aminosalicylates (5-ASAs): Medications like mesalamine are generally used for mild to moderate Crohn's affecting the colon, particularly Crohn's colitis. They work by reducing inflammation in the lining of the bowel.
- Corticosteroids: Drugs like prednisone are potent anti-inflammatory agents used for short-term control of severe flares. While highly effective in rapidly reducing inflammation, they come with significant side effects and are not suitable for long-term inflammatory bowel disease treatment.
- Immunomodulators:
- Azathioprine and Methotrexate: These medications work by suppressing the immune system, thereby reducing the inflammatory response. They are often used for maintenance therapy to keep Crohn's in remission and reduce the need for corticosteroids. They can take several weeks or months to become fully effective.
- Biologic Therapies: This represents a significant advancement in Crohn's disease treatment for moderate to severe cases. These drugs target specific proteins in the immune system that promote inflammation.
- Anti-TNF Agents (e.g., Infliximab, Adalimumab): These block Tumour Necrosis Factor-alpha (TNF- ), a key inflammatory protein.
- Vedolizumab: Targets specific immune cells in the gut, reducing inflammation with fewer systemic side effects.
- Ustekinumab: Blocks interleukins-12 and -23, other inflammatory proteins.
Biologics are usually administered via infusion or injection and have revolutionized managing Crohn's disease for many patients. - Antibiotics: Medications like metronidazole or ciprofloxacin may be used to treat bacterial overgrowth in the small intestine, or to address complications like abscesses and fistulas that can arise from Crohn’s disease.
Nutritional Therapy:
- Exclusive Enteral Nutrition (EEN): Particularly effective in children and adolescents, EEN involves consuming only a liquid formula for a period, providing complete nutrition while allowing the bowel to rest and heal. It can be as effective as corticosteroids in inducing remission.
Surgery:
- Surgery is not a cure for Crohn’s but is often necessary for patients who don't respond to medical therapy or develop complications.
- Bowel Resection: Involves removing the diseased section of the bowel and rejoining the healthy ends.
- Strictureplasty: A procedure to widen narrowed sections of the bowel (strictures) without removing a large segment.
Surgery can significantly improve quality of life for many patients, offering relief from severe Crohn's symptoms.
Q8: Is Crohn’s disease curable?
This is a question that weighs heavily on the minds of many patients and their families. The direct answer, unfortunately, is no – there is currently no known cure for Crohn’s disease. It is a chronic condition that, once diagnosed, requires ongoing management.
However, "no cure" does not mean "no hope" or "no relief." Far from it. With effective Crohn's disease treatment strategies, including the advanced medications and therapies mentioned above, it is entirely possible for patients to achieve long-term remission. Remission means that the inflammation in the digestive tract has subsided, and patients can live symptom-free for extended periods, sometimes even years. This is a crucial distinction and a significant achievement in managing Crohn's disease. Many individuals with Crohn's lead full, active, and productive lives, often forgetting they even have the condition for stretches of time.
The field of IBD research is dynamic, with ongoing investigations into new biologics, small molecule drugs, and even therapies like stem cell transplantation. These advancements offer promising avenues for more effective and potentially curative treatments in the future, providing hope for patients worldwide living with this inflammatory bowel disease.
Managing Crohn’s Disease Through Lifestyle & Diet
Q9: How can diet help in managing Crohn’s disease?
While diet doesn't cause Crohn’s disease, it plays a critical role in managing Crohn's disease and its symptoms, particularly during flare-ups. Proper nutrition can help reduce inflammation, promote healing, and ensure you receive essential nutrients, preventing malabsorption issues commonly associated with active disease. It’s like tending to a delicate garden; what you feed it makes all the difference.
Foods to generally consider:
- Low-Fiber Fruits: Ripe bananas, peeled apples, melon – these are easier to digest during a flare.
- Well-Cooked Vegetables: Steamed or boiled carrots, spinach, pumpkin – cooking breaks down fibers, making them less irritating.
- Lean Proteins: Fish, chicken (skinless), eggs, lentils (well-cooked and pureed) – essential for tissue repair and overall strength.
- Probiotics: Yogurt (dahi), kefir, buttermilk – if tolerated and not lactose intolerant, these can help balance the gut microbiome.
- Omega-3 Fatty Acids: Found in fatty fish like salmon, flaxseeds, walnuts – known for their anti-inflammatory properties.
Foods to generally limit or avoid during a flare-up:
- High-Fiber, Raw Vegetables and Fruits: Can be difficult to digest and exacerbate symptoms.
- High-Fat Foods: Fried snacks, rich curries, excessive oils – can trigger diarrhea and abdominal pain.
- Spicy Foods: Chillies, strong masalas – often irritate an inflamed gut.
- Processed Foods and Refined Sugars: Lack nutritional value and can contribute to gut inflammation.
- Dairy Products: If you're lactose intolerant, dairy can trigger symptoms.
- Alcohol and Caffeine: Can stimulate bowel movements and worsen dehydration.
Remember, dietary tolerance is highly individual. Maintaining a food diary can help identify personal trigger foods. For a deeper dive into gut-friendly eating, consider this excellent resource: 👉 Watch: Eat These Fantastic Foods for a Healthy Small Intestine! provided by the experts at Bangalore Gastro Centre, focusing on foods that can truly support your gut health as part of your inflammatory bowel disease treatment plan.
Q10: How does stress management help with Crohn’s disease?
It’s a common misconception that stress causes Crohn’s disease. This is not true. However, stress is undeniably a major trigger for Crohn's symptoms flare-ups. The gut and brain are intimately connected via the gut-brain axis, meaning emotional and psychological stress can directly impact gut function, exacerbating inflammation and leading to a worsening of symptoms. Picture it like this: your gut and brain are constantly having a conversation; when one is stressed, the other feels it.
Incorporating effective stress management techniques into your daily routine is an essential component of managing Crohn's disease. Here are some helpful strategies:
- Yoga and Meditation: Practices like Surya Namaskar or simple pranayama (breathing exercises) can significantly reduce stress and promote relaxation.
- Mindfulness: Focusing on the present moment can help reduce anxiety about future flare-ups.
- Adequate Sleep: Prioritizing 7-9 hours of quality sleep each night allows your body to rest and repair.
- Regular Exercise: Gentle activities like walking or swimming can be powerful stress relievers.
- Therapy or Counseling: Speaking with a therapist can provide coping mechanisms and support for managing the emotional toll of chronic illness.
By actively managing Crohn's disease through stress reduction, you empower yourself to have greater control over your condition and potentially decrease the frequency and intensity of flare-ups, thereby enhancing the effectiveness of your overall Crohn's disease treatment.
Q11: Why does stomach upset cause headache?
This is a question many people ponder, not just those with Crohn's. The connection between your stomach upset and a throbbing headache might seem counterintuitive, but it's a prime example of the powerful gut-brain connection. Our gut and brain are in constant communication, influencing each other's function. When there’s inflammation or an imbalance in your gut microbiome, as often happens with conditions like Crohn’s disease, this can send signals to the brain that contribute to headaches or even migraines. It's like a noisy neighbour disrupting the peace next door.
Beyond the direct gut-brain axis, other factors related to stomach upset, especially in the context of Crohn's disease, can contribute to headaches:
- Dehydration: Severe diarrhea, a common Crohn's symptom, can lead to significant fluid loss, resulting in dehydration, which is a frequent cause of headaches.
- Nutrient Malabsorption: Crohn's can impair the absorption of vital nutrients and electrolytes. Deficiencies in certain vitamins and minerals can trigger neurological symptoms, including headaches.
- Inflammatory Mediators: The chronic inflammation characteristic of inflammatory bowel disease releases various chemical messengers (cytokines) into the bloodstream, which can cross the blood-brain barrier and induce pain, including headaches.
This highlights why managing Crohn's disease and focusing on overall gut health is crucial for systemic wellness, extending beyond just digestive comfort. Addressing the root causes of stomach upset is often key to alleviating associated symptoms like headaches, reinforcing the holistic nature of Crohn's disease treatment. You might find this blog post on Gastroparesis relevant as it also touches upon stomach issues: Gastroparesis Treatment: Diet, Symptoms & Stomach Paralysis.
Crohn’s vs Ulcerative Colitis — What’s the Difference?
Q12: Crohn’s vs Ulcerative Colitis — how do they differ?
Often, when discussing Crohn's disease, its counterpart, ulcerative colitis, inevitably comes up. Both are types of inflammatory bowel disease, but they have distinct characteristics that differentiate them. Understanding these differences is crucial for accurate diagnosis and effective inflammatory bowel disease treatment. Think of them as two siblings from the same family (IBD) but with very different personalities and preferences.
Feature | Crohn's Disease | Ulcerative Colitis |
Location | Can affect any part of the GI tract, from mouth to anus. Most commonly affects the end of the small intestine (ileum) and the beginning of the large intestine (colon). | Affects only the colon and rectum. |
Inflammation Pattern | Patchy areas of inflammation, with healthy segments of bowel between diseased areas. | Continuous inflammation, starting in the rectum and extending upwards through the colon. |
Depth of Inflammation | Involves all layers of the bowel wall (transmural). This deep inflammation can lead to complications like fistulas and strictures. | Affects primarily the innermost lining (mucosa) of the colon. |
Microscopic Appearance | Granulomas (collections of immune cells) are often seen in biopsies. | No granulomas. |
Common Symptoms | Abdominal pain, persistent diarrhea, weight loss, fatigue, blood in stool (less common than UC). | Urgent diarrhea, rectal bleeding, abdominal pain, weight loss, fatigue. |
Complications | Fistulas, strictures, abscesses, bowel obstruction, perianal disease, malabsorption. | Toxic megacolon, increased risk of colorectal cancer (with long-standing disease). |
Surgical Treatment | Often requires surgery for complications, but disease can recur at surgical sites. | Colectomy (removal of the colon) is curative. |
While some Crohn's symptoms like abdominal pain and diarrhea overlap, the key differentiators lie in the location and pattern of inflammation. A colonoscopy with biopsies is the gold standard for distinguishing between these two forms of inflammatory bowel disease. This allows gastroenterologists to accurately assess the extent and characteristics of the inflammation, leading to a precise diagnosis and the most appropriate Crohn's disease treatment or ulcerative colitis management plan.
Long-Term Outlook and When to See a Gastroenterologist
Q13: What is the long-term outlook for someone with Crohn’s disease?
Receiving a diagnosis of Crohn's disease can be daunting, but it's crucial to remember that the long-term outlook is far more positive than it once was. With appropriate Crohn's disease treatment and consistent lifestyle adaptation, many individuals with Crohn's disease can lead full, active, and meaningful lives, much like managing other chronic conditions such as diabetes or hypertension. The goal is not just symptom control but achieving and maintaining remission, preventing disease progression and complications.
The importance of early diagnosis cannot be overstated. Catching the disease in its initial stages and initiating effective inflammatory bowel disease treatment helps prevent the development of severe complications like strictures (narrowing of the bowel), fistulas (abnormal connections between parts of the bowel or to other organs/skin), and chronic malnutrition.
Continuous care with a specialized gastroenterologist is paramount. These specialists play a vital role in monitoring the disease activity, assessing the effectiveness of managing Crohn's disease strategies, and tailoring medications as needed. Regular check-ups, follow-up colonoscopies, and blood tests are essential to track progress, detect any changes early, and adjust the Crohn's disease treatment plan to ensure optimal gut health.
Specialized gastro centres, like the Bangalore Gastro Centre, are equipped with advanced diagnostic tools and offer expertise in state-of-the-art endoscopic procedures and the latest biologic therapies. Such dedicated care ensures that patients receive the most comprehensive and individualized approach to managing Crohn's disease, empowering them to live their lives to the fullest.
Key Takeaways & Educational Resources
Navigating a chronic condition like Crohn's disease requires both patience and comprehensive knowledge. Here are the key takeaways from our discussion:
- Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the digestive tract, often causing patchy, deep inflammation.
- Recognizing Crohn's symptoms early is crucial, though they can often mimic other digestive issues, necessitating a thorough diagnosis.
- While there's no cure, effective Crohn's disease treatment through medications (including biologics), nutritional therapy, and sometimes surgery, allows many patients to achieve long-term remission and lead fulfilling lives.
- Managing Crohn's disease extends beyond medication to include significant lifestyle modifications, especially dietary choices and stress management, which can significantly reduce flare-ups.
- Understanding the differences between Crohn's and ulcerative colitis, and recognizing the gut-brain connection that links stomach upset to headaches, underscores the holistic nature of gut health.
- Regular check-ups with a gastroenterologist are essential for monitoring the disease and ensuring a tailored inflammatory bowel disease treatment plan for the best long-term outlook.
We encourage you to continue your journey of learning about digestive wellness. The experts at Bangalore Gastro Centre are dedicated to providing accessible and accurate information to help you manage your gut health effectively. For more expert insights, educational videos, and practical tips on managing various digestive conditions, we invite you to subscribe to our YouTube channel. Knowledge is power, especially when it comes to your health!
