Pancreatic Enzyme Deficiency: Symptoms, Causes & Treatment Options Explained by Experts
Imagine your digestive system as a highly efficient kitchen. Every ingredient needs to be properly chopped, diced, and prepared before it can be cooked and absorbed. In this culinary analogy, your pancreas is the master chef, responsible for sending out a crucial team of workers: pancreatic enzymes. These powerful digestive enzymes are the unsung heroes that break down the fat, protein, and carbohydrates from your food into smaller, absorbable units. Without them, even the most nutritious meal can become a source of discomfort rather than nourishment.
However, sometimes this master chef falls short, leading to a condition known as pancreatic enzyme deficiency. This occurs when your pancreas doesn't produce enough of these vital digestive enzymes. When this shortage is significant, it can lead to a more serious medical condition called exocrine pancreatic insufficiency (EPI), where your body struggles to digest food properly.
If your meals often leave you bloated, tired, or with unpredictable bowel movements, your pancreas might be trying to tell you something. Understanding this deficiency is the first step towards finding relief and improving your overall well-being. Let’s answer common patient questions about pancreatic enzyme deficiency to shed light on this often-misunderstood digestive challenge.
Understanding Pancreatic Enzyme Deficiency
Pancreatic enzyme deficiency is a condition that warrants a deeper look. Medically, it's often referred to as Exocrine Pancreatic Insufficiency (EPI), highlighting the exocrine function of the pancreas – its role in producing and secreting digestive enzymes into the small intestine. This isn't just a minor inconvenience; it significantly impacts your body's ability to extract nutrients from the food you eat.
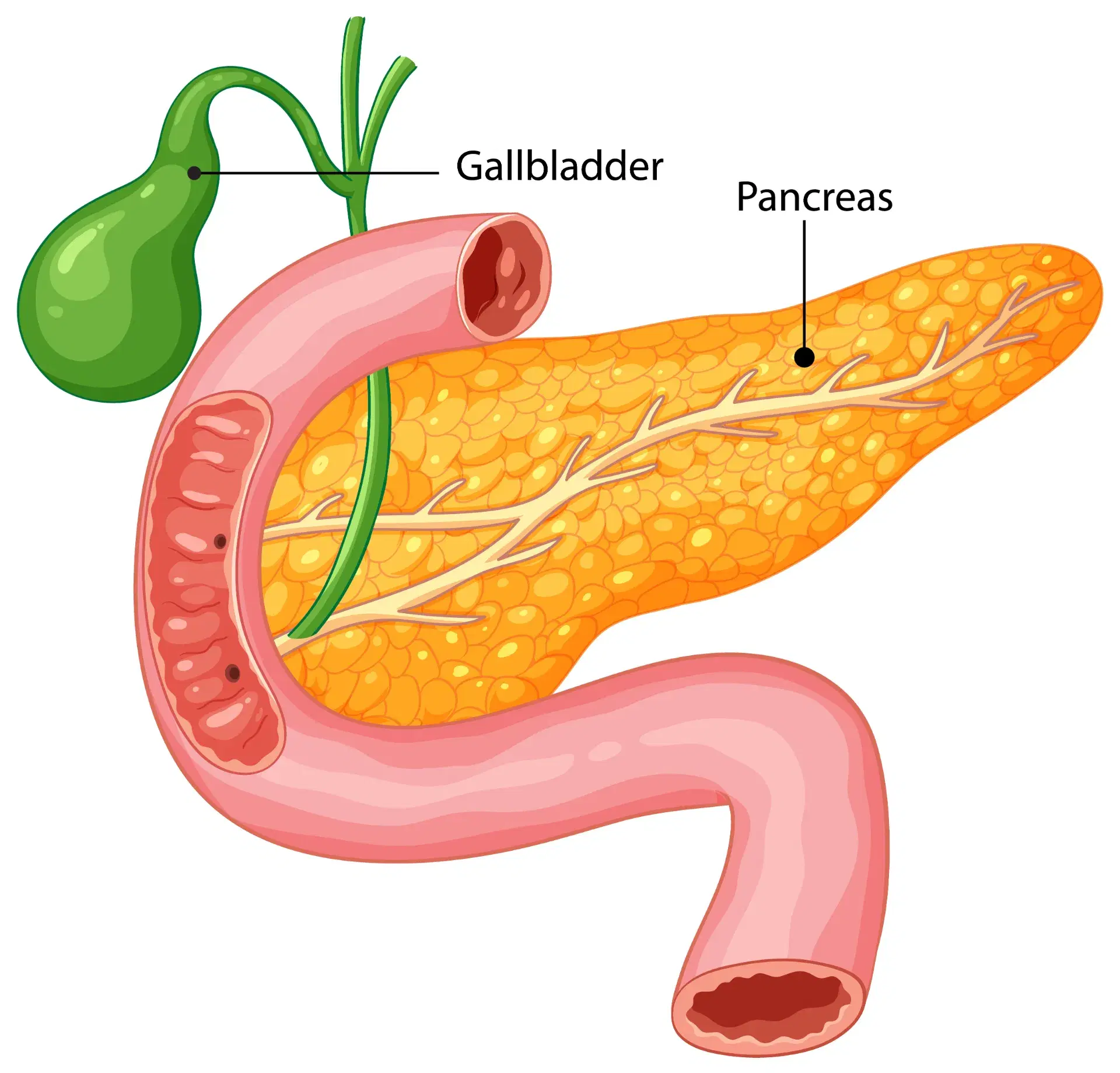
Several common causes can lead to EPI. Chronic pancreatitis, a persistent inflammation of the pancreas, is a leading culprit. Conditions like cystic fibrosis, diabetes, and even pancreatic surgery can also impair the pancreas's ability to produce enzymes. Sometimes, a blockage in the pancreatic duct, perhaps due to gallstones or a tumour, can prevent enzymes from reaching the small intestine, leading to pancreatic enzyme deficiency. The enzyme deficiency develops either because the pancreas itself is damaged and cannot produce enough enzymes, or because the secretion mechanism is compromised.
Your pancreas primarily churns out three major types of enzymes, each with a specific role:
- Lipase: This enzyme is crucial for breaking down fats. Without sufficient lipase, fats pass through your system undigested, leading to characteristic symptoms.
- Amylase: This is responsible for digesting complex carbohydrates, like starches, into simpler sugars that your body can absorb.
- Protease: This enzyme tackles proteins, breaking them down into amino acids, the building blocks for muscles and other bodily functions.
Early warning pancreatic insufficiency symptoms can include noticeable changes like oily stools (steatorrhea), which might float or be difficult to flush, often accompanied by a foul smell. Other common signs are persistent bloating, excessive flatulence, a feeling of constant fatigue, and unexplained weight loss despite eating regularly. This digestive enzymes shortage means your gut may not absorb nutrients properly, leading to malnutrition, which can manifest in various ways, from brittle hair and nails to a compromised immune system. These initial indicators often prompt further investigation into the health of your digestive system.
Q&A 1: Why Does Stomach Upset Cause Headache?
It might seem strange that a stomach upset could lead to a headache, but the human body is an intricate network where various systems are constantly communicating. This connection is often referred to as the "gut-brain axis," a two-way street between your digestive system and your brain. When you experience digestive distress, particularly from a pancreatic enzyme deficiency, it can indeed trigger a headache.
Here's how this fascinating connection works: When your body struggles with a digestive enzymes shortage, food isn't properly broken down and absorbed. This undigested food can ferment in your gut, leading to an overgrowth of harmful bacteria and an imbalance in your gut microbiome. This imbalance can produce toxins and inflammatory chemicals that don't stay confined to your gut. They can enter your bloodstream and, through various pathways, affect your nervous system, potentially triggering headaches. Think of it like a domino effect – one issue in your body setting off another far removed.
Furthermore, pancreatic insufficiency symptoms like persistent bloating and malabsorption can lead to dehydration or low energy levels, both of which are common triggers for headaches. Imagine feeling constantly parched or running on fumes – your head is often the first place to register this distress. If your body isn't absorbing essential nutrients like B vitamins and magnesium – crucial for nerve function and energy production – from your diet, it can also contribute to headaches. These nutrient deficiencies are a direct consequence of an untreated pancreatic enzyme deficiency.
Addressing the underlying digestive enzymes shortage and improving your gut health can often lead to a significant improvement in both your digestive comfort and the frequency and severity of your headaches. It’s a holistic approach that acknowledges the interconnectedness of your bodily systems. Learn more about how your digestive system affects your mood and energy [link to BGC blog on digestion habits].
So how do you know if you actually need extra enzymes to help digestion? Let's explore that next.
Q&A 2: How to Know If You Need Digestive Enzymes
Recognizing the need for digestive enzymes, specifically in the context of pancreatic enzyme deficiency, is crucial for maintaining good health. Many people experience occasional digestive discomfort, but when do these symptoms cross the line into indicating an enzyme shortage? You should start to suspect a digestive enzymes shortage if you experience chronic bloating, persistent gas, a feeling of excessive fullness after meals, or the characteristic greasy stools mentioned earlier. Fatigue after meals is another significant indicator, as your body expends more energy trying to process undigested food, leaving less for other activities.
There are several visible and non-visible signs that can point towards pancreatic insufficiency symptoms. Visible signs include:
- Steatorrhea: This is perhaps the most telling sign – pale, oily, voluminous, and foul-smelling stools that are difficult to flush. It’s a clear indication that fats are not being properly absorbed.
- Undigested food in stool: While not always indicative of EPI, seeing significant amounts of undigested food particles in your stool, especially after consuming fibrous vegetables, can be a sign.
- Unexplained weight loss: If you are losing weight despite maintaining a regular diet, it’s a red flag. Your body isn't absorbing the calories and nutrients it needs.
Non-visible signs can be equally debilitating:
- Constant fatigue: Even after a full night's sleep, you might feel drained due to poor nutrient absorption and the extra work your digestive system is doing.
- Poor nutrient absorption: This can lead to a host of problems, from vitamin deficiencies (especially fat-soluble vitamins A, D, E, K) to mineral imbalances, impacting everything from bone health to immunity.
- Brain fog: A feeling of mental sluggishness or difficulty concentrating can also be a consequence of nutrient deficiencies and the gut-brain axis at play.
Here’s a short checklist to help you gauge if you might need digestive enzymes:
- Are your stools consistently pale, oily, or floating?
- Do you feel uncomfortably full quickly or experience significant abdominal discomfort and bloating after most meals?
- Are you losing weight despite eating a normal or even increased amount of food?
- Do you frequently experience excessive gas or flatulence?
- Do you feel chronically tired or lack energy, especially after eating?
It's important to differentiate between a temporary digestive enzymes shortage, which might occur due to a temporary gut infection, acute stress, or as a natural part of aging, and true pancreatic enzyme deficiency (EPI). EPI is a more chronic condition arising from persistent pancreatic dysfunction. While over-the-counter enzyme supplements can offer temporary relief for general digestive woes, they are not a substitute for diagnosing and treating actual EPI. It is highly encouraged to consult a gastroenterologist before self-prescribing enzyme supplements. They can conduct specific diagnostic tests to determine the root cause of your symptoms, ensuring you receive appropriate and effective treatment, preventing further complications related to pancreatic enzyme deficiency.
Q&A 3: What Happens Without Pancreatic Enzymes?
The consequences of living with an untreated pancreatic enzyme deficiency can be far-reaching and significantly impact your quality of life. Without enough pancreatic enzymes, the most fundamental process of digestion – breaking down food into usable nutrients – grinds to a halt. Food simply isn't broken down properly, leading to severe nutrient malabsorption. It's like having a car with a full fuel tank but no engine to convert that fuel into power.
Let's break down the impact on each macronutrient:
- Fats: This is where the most noticeable problems arise. Without sufficient lipase, fats remain undigested, leading to the characteristic oily, foul-smelling stools (steatorrhea). More critically, the malabsorption of fats also means your body can't absorb fat-soluble vitamins – A, D, E, and K. Deficiencies in these vitamins can lead to a myriad of health issues, from impaired vision (Vitamin A) and weak bones (Vitamin D) to blood clotting problems (Vitamin K) and compromised immunity.
- Proteins: A lack of protease means proteins aren't broken down into amino acids. This can result in muscle loss, general weakness, and a reduced capacity for tissue repair and growth. You might notice your muscles feeling flabbier or your energy levels consistently low.
- Carbohydrates: While typically less severe than fat malabsorption, a shortage of amylase can lead to carbohydrates passing undigested into the large intestine. Here, they ferment, causing significant bloating, excessive gas, and sometimes diarrhea.
The long-term effects of untreated exocrine pancreatic insufficiency are grave. Chronic malnutrition becomes a serious concern, affecting every system in your body. Your immune system can become weakened, making you more susceptible to infections. Bone health can suffer, leading to osteoporosis due to poor calcium and Vitamin D absorption. Anemia, caused by iron and B12 deficiencies, can leave you feeling constantly tired and weak.
Beyond the physical, there are significant emotional and social effects. The constant abdominal discomfort, unpredictable bowel movements, and fatigue can lead to frustration, anxiety, and even depression. Many individuals begin to avoid social eating situations, further isolating them. This is where pancreatic enzyme replacement therapy (PERT) becomes a game-changer, as it can restore proper digestion, alleviate these symptoms, and significantly improve a patient's overall well-being. Learn how enzyme therapy helps people with chronic pancreatitis [https://www.bangaloregastrocentre.com/].
But can your pancreas ever bounce back on its own? This is a common and important question.
Q&A 4: Can Pancreatic Function Improve?
The question of whether pancreatic function can improve when facing a pancreatic enzyme deficiency is a hopeful one, and the honest, evidence-based answer is: it depends heavily on the underlying cause and the extent of the damage.
In cases of mild or early-stage exocrine pancreatic insufficiency, particularly when the cause is reversible or manageable, pancreatic function can indeed see significant improvement. This might occur with prompt treatment of the underlying condition, coupled with crucial lifestyle changes, and effective inflammation control. For instance, if the deficiency is linked to acute pancreatitis that resolves without extensive scarring, or if it's due to a treatable blockage, there's a good chance for recovery of some pancreatic enzyme production. Early diagnosis and intervention are key here.
However, in chronic conditions, such as advanced chronic pancreatitis, where there's irreversible damage and fibrosis (scarring) of the pancreatic tissue, the loss of enzyme-producing cells may be permanent. In such scenarios, while the lost function may not fully return, the symptoms can be very effectively managed, and further deterioration can often be prevented. This is a critical distinction – improvement in managing symptoms and preserving remaining function versus a complete restoration of the pancreas to its original state.
Crucial lifestyle modifications play a significant role in preserving residual pancreatic function and supporting overall pancreatic health. Adopting a balanced, healthy diet (as we’ll discuss later), completely quitting alcohol and smoking, and diligently treating any underlying diseases (like diabetes or autoimmune conditions that affect the pancreas) can help reduce the strain on the pancreas and protect its remaining enzyme-producing capacity. For many individuals with significant pancreatic enzyme deficiency, Pancreatic Enzyme Replacement Therapy (PERT) is introduced as a cornerstone treatment. This therapy doesn't improve the pancreas's own function, but rather supplements the body with the enzymes it can no longer produce, thereby controlling symptoms and preventing malnutrition.
The scientific community is also actively researching avenues for pancreatic regeneration and the role of gut microbiome support in improving pancreatic health. While these are promising areas, for now, managing symptoms and supporting existing function remain the primary focus. Understanding the limits and possibilities of pancreatic recovery is vital for patients and clinicians alike when addressing exocrine pancreatic insufficiency.
Diagnosis and Medical Evaluation
Accurate diagnosis of pancreatic enzyme deficiency is the critical first step towards effective treatment and relief. When you suspect pancreatic insufficiency symptoms, consulting a healthcare professional, especially a gastroenterologist, is paramount. They employ a combination of tests and clinical evaluation to confirm the diagnosis and identify the underlying cause.
One of the most common and reliable diagnostic tests is the Fecal Elastase-1 Test. This non-invasive stool test measures the amount of elastase, a specific enzyme produced solely by the pancreas. Low levels of fecal elastase-1 strongly confirm pancreatic enzyme deficiency. It's a simple, yet highly effective way to assess pancreatic exocrine function.
Another test that might be used is Stool Fat Quantification, often referred to as a 72-hour fecal fat test. This test measures the amount of fat excreted in your stool over three days. Elevated fat levels (steatorrhea) are a clear indication of fat malabsorption, which is a hallmark of EPI.
Beyond stool tests, imaging studies play a vital role in assessing the structure of your pancreas. CT scans (Computed Tomography) and MRI (Magnetic Resonance Imaging) can reveal signs of chronic pancreatitis, such as calcifications, ductal changes, or atrophy of the pancreas. Sometimes, more specialized imaging like Endoscopic Ultrasound (EUS) might be performed for a detailed view of the pancreatic ducts and surrounding tissues.
At a gastroenterology appointment, you can expect a thorough discussion of your medical history, symptoms, and lifestyle habits. The doctor will likely perform a physical examination and order the necessary blood tests to check for nutritional deficiencies. Emphasizing the role of expert evaluation at specialized centres like Bangalore Gastro Centre is important for accurate diagnosis and tailored treatment plans. These centres often have the advanced diagnostic tools and experienced specialists to pinpoint the exact cause of your pancreatic enzyme deficiency, whether it's chronic pancreatitis, diabetes, gallstones, or another condition. Identifying the underlying cause is crucial because treating it can sometimes alleviate or improve the enzyme deficiency.
Treatment Options: Pancreatic Enzyme Replacement Therapy (PERT)
Once pancreatic enzyme deficiency is diagnosed, the primary and most effective treatment is Pancreatic Enzyme Replacement Therapy (PERT). This therapy is a lifeline for many patients suffering from exocrine pancreatic insufficiency, providing the crucial enzymes that their own pancreas can no longer produce in sufficient quantities.
So, what is PERT and how does it work? Simply put, PERT involves taking prescription medications that contain a mixture of lipase, amylase, and protease – essentially, synthetic versions of the enzymes your pancreas should be making. When you take these capsules with your meals, these enzymes mix with your food in the stomach and travel to the small intestine, where they go to work, breaking down fats, proteins, and carbohydrates, just as your natural enzymes would. This process allows for proper nutrient absorption, alleviating the debilitating pancreatic insufficiency symptoms and preventing malnutrition.
Taking enzymes correctly is vital for their effectiveness. PERT medications are typically taken with every meal and snack that contains fat, protein, or carbohydrates. The dosage is highly individualized and depends on the severity of your deficiency, the fat content of your meal, and your body's response. Most PERT capsules are enteric-coated, meaning they have a special coating that prevents stomach acid from inactivating the enzymes before they reach the small intestine. This is why it's important not to crush or chew the capsules unless specifically instructed by your doctor, as this can destroy the coating and render the enzymes ineffective. Common enzyme brands are available, and your doctor will prescribe the most suitable one for your condition.
Monitoring and dosage adjustments are an ongoing part of PERT. Your doctor will assess your symptoms – such as the presence of oily stools, bloating, and weight changes – to fine-tune your dosage. The goal is to find the right balance that allows for optimal digestion and symptom control.
In addition to PERT, adjunct treatments might be recommended. This can include taking fat-soluble vitamin supplements (A, D, E, K) because of the long-term malabsorption. Probiotics may be suggested to support a healthy gut microbiome. Eating smaller, more frequent meals can also help reduce the burden on your digestive system. Bangalore Gastro Centre plays an educational role in helping patients understand the nuances of therapy adherence, emphasizing the importance of consistent and correct use of pancreatic enzyme replacement for long-term health and symptom management.
Dietary & Lifestyle Support
While Pancreatic Enzyme Replacement Therapy (PERT) is often the cornerstone of treatment for pancreatic enzyme deficiency, dietary and lifestyle adjustments play a crucial supportive role. These changes can significantly alleviate pancreatic insufficiency symptoms, enhance the effectiveness of enzyme therapy, and promote overall digestive wellness.
Here are some key diet tips for pancreatic health and managing a digestive enzymes shortage:
- Eat Small, Balanced Meals: Instead of three large meals, opt for 5-6 smaller, more frequent meals throughout the day. This reduces the digestive load on your system, allowing the enzymes (both natural and supplemental) to work more efficiently.
- Rich in Lean Protein and Whole Grains: Focus on easily digestible lean proteins like chicken, fish, lentils, and paneer. Incorporate whole grains like oats, brown rice, and whole wheat bread, which provide sustained energy and fiber without being overly taxing on the digestive system.
- Limit Alcohol, Fried Foods, and Processed Fats: These are notorious for triggering pancreatic stress and exacerbating symptoms. Alcohol can directly damage pancreatic cells, while excessive fats, especially unhealthy trans fats found in fried and processed foods, are difficult to digest and put a heavy burden on your lipase enzymes. Think of traditional Indian snacks like samosas and pakoras; while delicious, they should be consumed in moderation or avoided if they trigger symptoms.
- Stay Hydrated: Drinking plenty of water throughout the day aids digestion and prevents constipation, a common issue when digestion is compromised.
- Balance Fiber Intake: While fiber is generally good for gut health, too much insoluble fiber can sometimes accelerate gut transit, potentially reducing the time for enzymes to work. Focus on a balanced intake of both soluble (found in oats, apples, lentils) and insoluble fiber (whole grains, vegetables).
The importance of nutrient-rich foods cannot be overstated. Opt for plenty of fruits, vegetables, and lean protein sources. These foods provide essential vitamins, minerals, and antioxidants that support overall health and help repair any damage caused by malnutrition. Good gut foods, such as those rich in prebiotics (garlic, onions, bananas) and probiotics (yogurt, kefir, idli/dosa batter), can help cultivate a healthy gut microbiome, which in turn can indirectly enhance enzyme activity and reduce inflammation within the digestive tract. These dietary strategies, combined with proper pancreatic enzyme replacement, form a powerful approach to managing pancreatic enzyme deficiency.
Eat These Fantastic Foods for a Healthy Small Intestine!
For readers eager to dive deeper into improving their gut function naturally, we highly recommend watching this informative video from Bangalore Gastro Centre. A healthy small intestine is crucial not just for nutrient absorption, but also for supporting better enzyme action and overall digestive efficiency. The video offers practical, expert advice on dietary choices that can make a real difference. Watch this video by Bangalore Gastro Centre’s experts to discover foods that can help your digestive system thrive.
When to Consult a Gastroenterologist
Understanding the signs that warrant professional medical attention is crucial, especially when dealing with potential pancreatic enzyme deficiency. While occasional digestive upsets are common, persistent and worsening symptoms should never be ignored. Early intervention is key to preventing long-term complications like malnutrition and irreversible organ damage.
Here are specific signs that indicate it’s time to consult a gastroenterologist:
- Persistent Bloating, Oily Stools, or Unexplained Weight Loss: If these pancreatic insufficiency symptoms continue for more than a few weeks, despite dietary adjustments, it’s a strong indicator that something more significant might be going on. Oily, foul-smelling stools, particularly, are a red flag for fat malabsorption.
- Chronic Fatigue Despite a Good Diet: If you consistently feel drained and tired, even when you believe you're eating nutritious food, it could be a sign that your body isn't absorbing the vital nutrients it needs due to a digestive enzymes shortage.
- Symptoms Worsening Even After Lifestyle Changes: If you've tried making dietary modifications and adopting healthier habits, but your digestive issues persist or intensify, it’s imperative to seek expert medical advice.
- New or Worsening Abdominal Pain: Any new onset or escalating abdominal pain, especially if it’s chronic or severe, should prompt an immediate visit to a specialist.
- Recurrent Diarrhea or Constipation: While these can have many causes, when combined with other symptoms of malabsorption, they warrant investigation.
Emphasizing early intervention cannot be overstated. Delaying diagnosis and treatment for pancreatic enzyme deficiency can lead to severe malnutrition, which impacts every bodily system, from immunity to bone density. The expert gastroenterology team at Bangalore Gastro Centre is equipped with the knowledge and technology to accurately diagnose and manage complex digestive disorders. They can provide a tailored treatment plan, whether it involves pancreatic enzyme replacement or other interventions. Don't hesitate to seek help if you suspect you might be experiencing pancreatic enzyme deficiency; your long-term health depends on it.
Conclusion
In summary, pancreatic enzyme deficiency, often manifesting as Exocrine Pancreatic Insufficiency (EPI), is a significant digestive challenge where your body struggles to break down and absorb nutrients effectively. From the distinct pancreatic insufficiency symptoms like oily stools and persistent bloating to systemic issues like fatigue and malnutrition, the impact on quality of life can be profound. However, the good news is that with early and accurate diagnosis, and proper treatment – primarily through Pancreatic Enzyme Replacement Therapy (PERT) – individuals can experience a drastic improvement in their health and well-being.
Reinforcing the importance of professional medical evaluation is paramount; self-diagnosis and self-treatment of a digestive enzymes shortage can lead to serious health complications. A balanced, nutrient-rich diet, coupled with appropriate medical intervention, forms the backbone of effective management. Empower yourself with knowledge to take charge of your digestive health journey.
